By Ellen Barry | The New York Times
Special thanks to Japantimes.com for making this article available

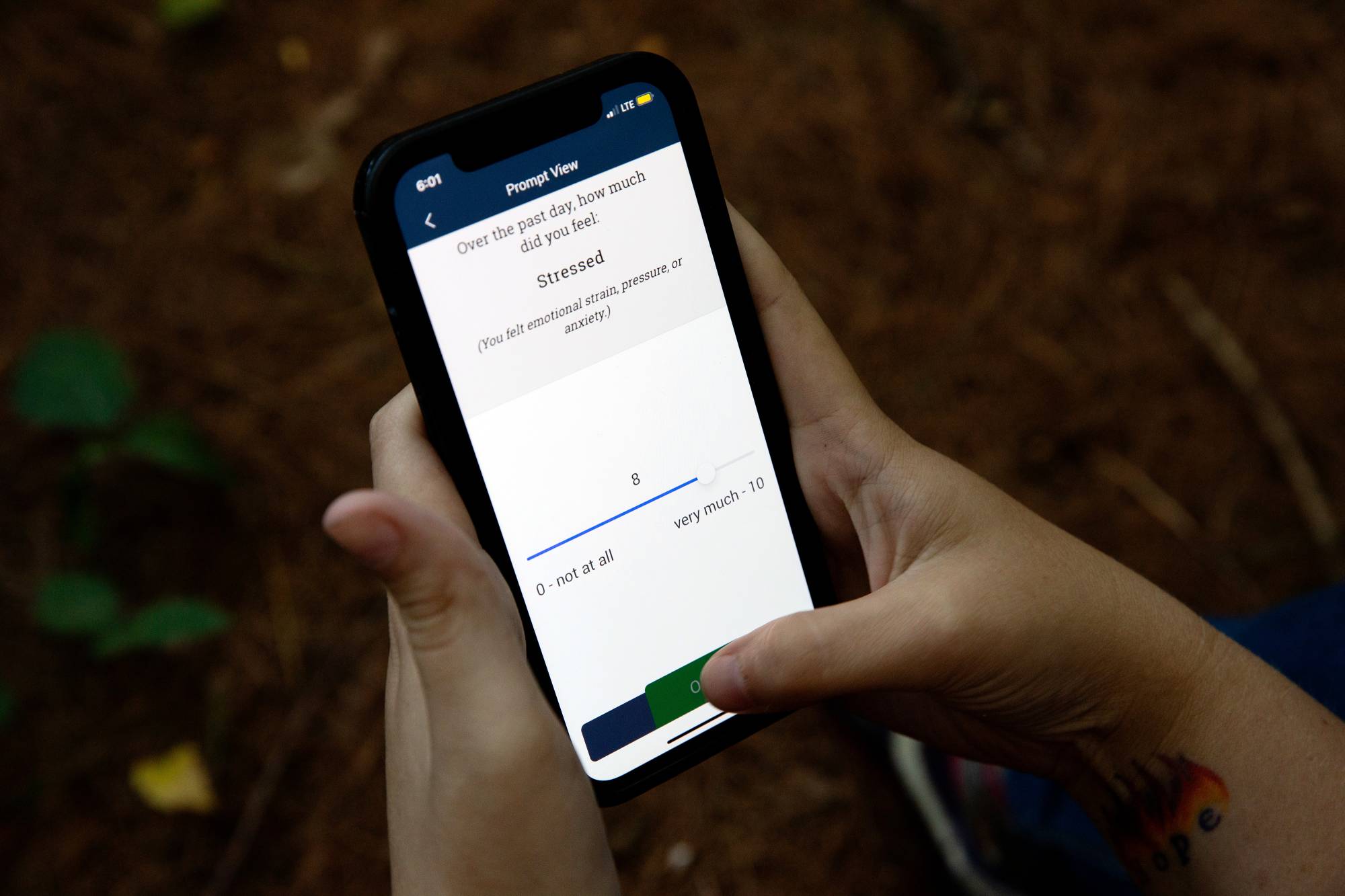
Katelin Cruz at a park near her home in Ware, Mass., on Sept. 1, 2022. Cruz uses a phone and FitBit to submit data about her mood and other metrics to Harvard researchers studying suicidal tendencies. (Kayana Szymczak/The New York Times)
CAMBRIDGE, MASSACHUSETTS – In March, Katelin Cruz left her latest psychiatric hospitalization with a familiar mix of feelings. She was, on the one hand, relieved to leave the ward, where aides took away her shoelaces and sometimes followed her into the shower to ensure that she would not harm herself.
But her life on the outside was as unsettled as ever, she said in an interview, with a stack of unpaid bills and no permanent home. It was easy to slide back into suicidal thoughts. For fragile patients, the weeks after discharge from a psychiatric facility are a notoriously difficult period, with a suicide rate around 15 times the national rate, according to one study.
This time, however, Cruz, 29, left the hospital as part of a vast research project which attempts to use advances in artificial intelligence to do something that has eluded psychiatrists for centuries: to predict who is likely to attempt suicide and when that person is likely to attempt it, and then, to intervene.
On her wrist, she wore a Fitbit programmed to track her sleep and physical activity. On her smartphone, an app was collecting data about her moods, her movement and her social interactions. Each device was providing a continuous stream of information to a team of researchers on the 12th floor of the William James Building, which houses Harvard University’s psychology department.
In the field of mental health, few new areas generate as much excitement as machine learning, which uses computer algorithms to better predict human behavior. There is, at the same time, exploding interest in biosensors that can track a person’s mood in real time, factoring in music choices, social media posts, facial expression and vocal expression.
Matthew K. Nock, a Harvard psychologist who is one of the nation’s top suicide researchers, hopes to knit these technologies together into a kind of early-warning system that could be used when an at-risk patient is released from the hospital.
He offers this example of how it could work: The sensor reports that a patient’s sleep is disturbed, she reports a low mood on questionnaires and GPS shows she is not leaving the house. But an accelerometer on her phone shows that she is moving around a lot, suggesting agitation. The algorithm flags the patient. A ping sounds on a dashboard. And, at just the right time, a clinician reaches out with a phone call or a message.
There are plenty of reasons to doubt that an algorithm can ever achieve this level of accuracy. Suicide is such a rare event, even among those at highest risk, that any effort to predict it is bound to result in false positives, forcing interventions on people who may not need them. False negatives could thrust legal responsibility onto clinicians.
Algorithms require granular, long-term data from a large number of people, and it’s nearly impossible to observe large numbers of people who die by suicide. Finally, the data needed for this kind of monitoring raises red flags about invading the privacy of some of society’s most vulnerable people.
Nock is familiar with all these arguments but has persisted, in part out of sheer frustration. “With all due respect to people who’ve been doing this work for decades, for a century, we haven’t learned a great deal about how to identify people at risk and how to intervene,” he said. “The suicide rate now is the same it was literally 100 years ago. So just if we’re being honest, we’re not getting better.”
A fire hose of data
On an August afternoon in the William James building, a lanky data scientist named Adam Bear sat in front of a monitor in Nock’s lab, wearing flip-flops and baggy shorts, staring at the zigzagging graphs of a subject’s stress levels over the course of a week.
When moods are mapped as data, patterns emerge, and it’s Bear’s job to look for them. He spent his summer poring through the days and hours of 571 subjects who, after seeking medical care for suicidal thoughts, agreed to be tracked continuously for six months. While they were being tracked, two died by suicide and between 50 and 100 made attempts.
It is, Nock believes, the largest reservoir of information ever collected about the daily lives of people struggling with suicidal thoughts.
The team is most interested in the days preceding suicide attempts, which would allow time for intervention. Already, some signs have emerged: Although suicidal urges often do not change in the period before an attempt, the ability to resist those urges does seem to diminish. Something simple — sleep deprivation — seems to contribute to that.
Nock has been looking for ways to study these patients since 1994, when he had an experience that shocked him profoundly. During an undergraduate internship in the United Kingdom, he was assigned to a locked unit for violent and self-injurious patients. There, he saw things he had never encountered: Patients had cuts up and down their arms. One of them pulled out his own eyeball. A young man he befriended, who seemed to be improving, was later found in the Thames.
Another shock came when he began to pepper the clinicians with questions about treating these patients and realized how little they knew: He recalls being told, “We give them some medicine, we talk to them and we hope they get better.”

One reason, he concluded, was that it had never been possible to study a large number of people with suicidal ideation in the same way that we are able to observe patients with heart disease or tuberculosis. “Psychology hasn’t advanced as much as other sciences because we’ve been largely doing it wrong,” he said. “We haven’t gone out and found some behavior that is important in nature, and gone out and observed it.”
But with the advent of phone-based apps and wearable sensors, he added, “we have data from so many different channels, and we have, increasingly, the ability to analyze those data, and observe people as they’re out living their lives.” One dilemma in designing the study was what to do when participants expressed a strong desire to hurt themselves. Nock decided they should intervene.
Telling the truth to a computer
It was around 9 p.m., a few weeks into the six-month study, when the question popped up on Cruz’s phone: “Right now how strong is your desire to kill yourself?”
Without stopping to think, she dragged her finger all the way to the end of the bar: 10. A few seconds later, she was asked to choose between two statements: “I am definitely not going to kill myself today” and “I am definitely going kill myself today.” She scrolled to the second.
Fifteen minutes later, her phone rang. It was a member of the research team calling her. The woman called 911 and kept Cruz on the line until police knocked on her door, and she passed out. Later, when she regained consciousness, a medical team was giving her a sternum rub, a painful procedure used to revive people after overdoses.
Cruz has a pale, seraphic face and a fringe of dark curls. She had been studying for a nursing degree when a cascade of mental health crises sent her life swerving in a different direction. She maintains an A-student’s nerdy interest in science, joking that the rib cage on her T-shirt is “totally anatomically correct.”
Right away, she had been intrigued by the trial, and she responded dutifully six times a day, when the apps on her phone surveyed her about her suicidal thoughts. The pings were intrusive, but also comforting. “It felt like I wasn’t being ignored,” she said. “To have somebody know how I feel, that takes some of the weight off.”
On the night of her attempt, she was alone in a hotel room in Concord, Massachusetts. She didn’t have enough money for another night there, and her possessions were mounded in trash bags on the floor. She was tired, she said, “of feeling like I had nobody and nothing.” Looking back, Cruz said she thought the technology — its anonymity and lack of judgment — made it easier to ask for help.
“I think it’s almost easier to tell the truth to a computer,” she said.
Last week, as the six-month clinical trial came to an end, Cruz filled out her final questionnaire with a twinge of sorrow. She would miss the $1 she received for each response. And she would miss the sense that someone was watching her, even if it was someone faceless, at a distance, through a device.
“Honestly, it makes me feel a little bit safer to know that somebody cares enough to read that data every day, you know?” she said. “I’ll be kind of sad when it’s over.”
This article originally appeared in The New York Times. © 2022 The New York Times Company
If you or someone you know is in crisis and needs help, resources are available. In case of an emergency in Japan, please call 119 for immediate assistance. The TELL Lifeline is available for those who need free and anonymous counseling at 03-5774-0992. For those in other countries, visit International Suicide Hotlines for a detailed list of resources and assistance.
