
The treatment options offered to patients with eating disorders in real-world settings largely depend on the judgment and training of clinicians and local constraints on which treatments can be provided. Unfortunately, few of these treatments are based on scientific evidence, and even fewer have been evaluated in clinical trials.
There is a consensus that the outpatient setting is the mainstay of treating eating disorders. It is less expensive and disruptive than day-hospital and inpatient treatments. However, some patients do not respond to the best available outpatient treatments. The most common option in these cases is to provide them with a more intensive form of care to improve their chances of recovery.
However, it is common for patients being transferred from a less intensive (e.g., outpatient) to a more intensive form of care (e.g., day-hospital or inpatient) and vice versa, to be treated with different treatment strategies and procedures in terms of theory and content. This approach produces discontinuities in the treatment process and may confuse patients about the procedures and strategies they should use to address their eating disorders.
The two main problems above indicate the need to promote the implementation of evidence-based treatment in standard clinical settings and the process of patient transfer from outpatient to intensive settings and vice versa.
Multistep enhanced cognitive behavior therapy (CBT-E): rationale and overview
The NICE guideline recommends cognitive behavior therapy for eating disorders (CBT-ED) as an evidence-based treatment for all eating disorders. CBT-E (E= ‘enhanced’) is one major example of the specialist cognitive-behavioral therapies for eating disorders covered by the umbrella term ‘CBT-ED’. CBT-E was initially developed to address eating disorder psychopathology (rather than the DSM diagnosis) of adult outpatients, but later it was also adapted for adolescents and intensive levels of care (i.e., day-hospital and residential and inpatient treatment).
The rationale behind extending CBT-E to intensive settings was based on three main considerations. First, a subgroup of patients fails to respond to outpatient CBT-E or have an eating disorder of such clinical severity that they cannot be managed safely in an outpatient setting. Second, data on changing the type of outpatient treatment in patients who are not responding to CBT-ED are inconclusive and only assessed in bulimia nervosa. In these cases, at least for anorexia nervosa, the alternative to outpatient treatment is often hospitalization in specialized eating disorder units, which generally adopts an eclectic approach not driven by a single empirically supported theory. Third, the ineffectiveness of outpatient CBT-E in some patients may depend on insufficient intensive care rather than the nature of the treatment itself.
CBT-E, having to be designed to treat all diagnostic categories of clinical eating disorders both in adults and adolescents in different settings of care (from outpatient to inpatient), offers the concrete possibility, for the first time in the field of evidence-based psychotherapy for eating disorders, to implement a stepped-care approach in real-world clinical settings overcoming some of the difficulties encountered in more conventional, fragmented clinical services. Indeed, the most distinctive feature of this approach, also termed multistep CBT-E, is that the same theory and procedures are applied at each level of care, as the main difference between the various steps is the intensiveness of treatment (see Figure 1).
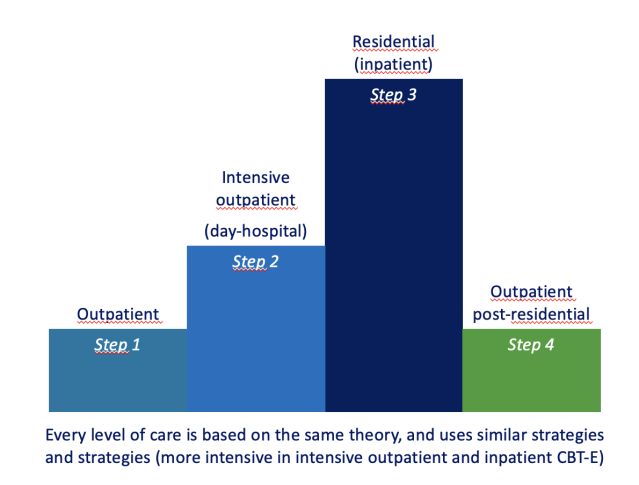
Figur1. The main steps of Multistep CBT-E
Riccardo Dalle Grave, MD
With this approach, non-responders to outpatient treatment and those whose physical conditions do not warrant hospitalization but who would benefit from more support can be offered a more intensive form of therapy within the CBT-E framework. Thus, patients can be moved seamlessly from outpatient care to residential care and then on to the final phase of outpatient treatment with no change in the nature of the treatment itself.
Most patients are initially treated as outpatients. As treatment unfolds, a patient’s progress is continually monitored, and should there be no measurable improvement after a reasonable period, the patient is encouraged to step up to intensive CBT-E. As the treatment intensiveness is stepped up in patients requiring specialist care, it is stepped down when they show concrete signs of improvement. Thus, outpatient CBT-E is offered to all patients completing intensive CBT-E.
In this way, CBT-E, implemented according to the stepped-care philosophy, aims to provide the maximum benefit to patients while minimizing the financial burden of their treatment without changing the treatment’s theory and content along the way. It is hoped that this “standardization” of approach will improve the chances for recovery in these patients, as it would avoid subjecting them to confusing and counter-productive changes in the therapeutic approach that commonly accompany such transitions.
This approach was first developed by my team in Garda, Verona (Italy), but similar services are also being set up in other European countries.
The Multistep CBT-E team
Multistep CBT-E is delivered by a “non-eclectic” multidisciplinary team in which all members (i.e., psychologists, dietitians, physicians) receive extensive training on CBT-E and are aware of the entire clinical picture of patients. In this non-eclectic multidisciplinary team, the dietitian’s intervention to address underweight and dietary restriction and the physician’s management of coexisting mental and general medical disorders (e.g., clinical depression, diabetes) or complications associated with eating disorders are integrated consistently with CBT-E
Advantages of a consistent intervention at different levels of care
A cross-level clinical service based on CBT-E has two main advantages. First, patients are treated with a single, well-delivered, evidence-based treatment rather than the evidence-free eclectic approach common elsewhere. Second, it minimizes the problems associated with transitions from outpatient to intensive treatment, as it avoids subjecting patients to the confusing and counterproductive changes in the therapeutic approach that commonly accompany such transitions. However, a different form of treatment must be offered to patients who do not respond to CBT-E.
Data on efficacy and effectiveness
The efficacy of outpatient CBT-E has been confirmed in adults with anorexia nervosa and bulimia nervosa, or other non-underweight eating disorders. Outpatient CBT-E has also achieved promising outcomes for adolescents with anorexia nervosa and bulimia nervosa.
The promising effect of Multistep CBT-E is supported by a study that tested the effectiveness of intensive CBT-E, previously only trialed in outpatients, in a group of 80 hospitalized patients with severe anorexia nervosa. The results showed that the treatment substantially improved weight, eating disorder features, and general psychopathology in these patients and attenuated the weight loss that typically follows hospitalization for anorexia nervosa.
References
Dalle Grave, R., Multistep cognitive behavioral therapy for eating disorders: Theory, practice, and clinical cases. Jason Aronson: New York, 2013.
Dalle Grave, R.; Calugi, S., A Young Person’s Guide to Cognitive Behaviour Therapy for Eating Disorders. Routledge: London, 2024.
Dalle Grave , R.; el Khazen, C., Cognitive behaviour therapy for eating disorders in young people: a parents’ guide. Routledge: London, 2022.
Dalle Grave, R.; Conti, M.; Calugi, S., Effectiveness of intensive cognitive behavioral therapy in adolescents and adults with anorexia nervosa. Int. J. Eat. Disord., 2020, 53 (9), 1428-1438.
