Recover Research Institute
Science has come a long way in helping us understand the way the brain changes in addiction. In this section, we will provide updates of current research on addiction, recovery, and the brain. CLICK TO LEARN MORE ABOUT: NEUROTRANSMITTERS, AGONISTS, & ANTAGONISTS
3 Key Points to Understand the Brain and Addiction:
1. Some characteristics of addiction are similar to other chronic diseases.
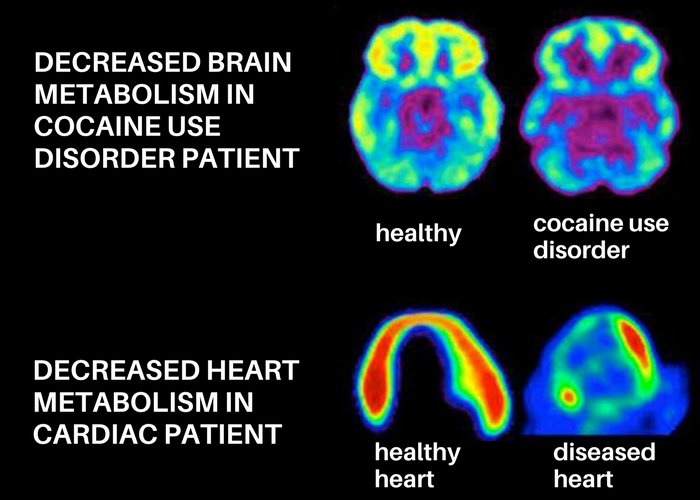
Just as cardiovascular disease damages the heart and changes its functioning, addiction changes the brain and impairs the way it works. Below is an image of the brain (left) and the heart (right).
These images show how scientists can use imaging technology to measure functioning of the brain and heart. Greater activity is shown in reds and yellows, and reduced activity is shown in blues and purples. Both the healthy brain and the healthy heart show greater activity than the diseased brain and heart, because both addiction and heart disease cause changes in function. In drug addiction, the frontal cortex in particular shows less activity. This is the part of the brain associated with judgment and decision-making (NIDA).
Addiction is similar to other chronic diseases in the following ways:
- It is preventable
- It is treatable
- It changes biology
- If untreated, it can last a lifetime
2. Substances of misuse trick the brain’s reward system.
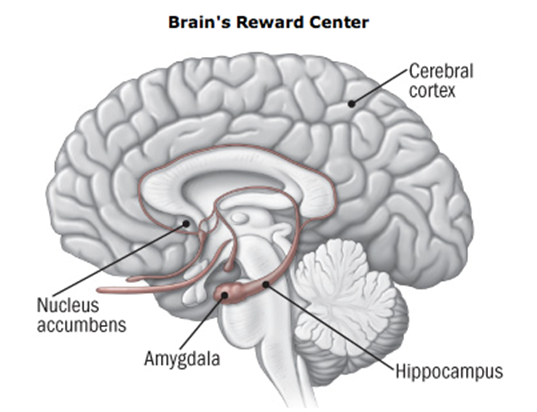
The brain can experience pleasure from all sorts of things we like to do in life; eat a piece of cake, have a sexual encounter, play a video game. The way the brain signals pleasure is through the release of a neurotransmitter (a chemical messenger) called dopamine into the nucleus accumbens, the brain’s pleasure center. This is generally a good thing; it ensures that people will seek out things needed for survival. But drugs of misuse, such as nicotine, alcohol, and heroin, also cause the release of dopamine in the nucleus accumbens, and in some cases these drugs cause much more dopamine release than natural, non-drug rewards.
Below is a picture (helpguide.org) of the brain and the nucleus accumbens, in addition to some other brain regions that are affected by addition.
The brain’s nucleus accumbens activated by alcohol (Gilman et al., 2008)
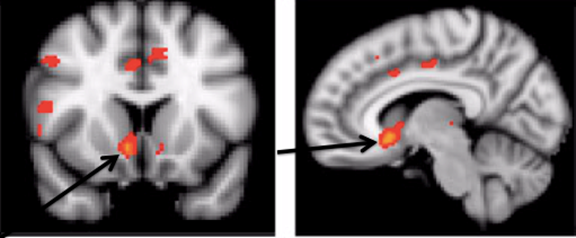
Addictive drugs can provide a shortcut to the brain’s reward system by flooding the nucleus accumbens with dopamine. Additionally, addictive drugs can release 2 to 10 times the amount of dopamine that natural rewards do, and they do it more quickly and reliably.
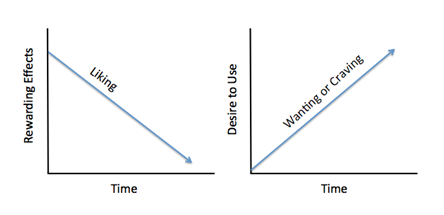
Over time, drugs become less rewarding, and craving for the drug takes over. The brain adapts to the effects of the drug (an effect known as tolerance), and because of these brain adaptations, dopamine has less impact. People who develop an addiction find that the drug no longer gives them as much pleasure as it used to, and that they have to take greater amounts of the drug more frequently to feel high.
There is a distinction between liking and wanting the drug; over time, the liking decreases and the wanting increases. Individuals with a substance use disorder continue to seek and use the substance, despite the negative consequences and tremendous problems caused for themselves and for their loved ones, because the substance allows them to simply feel normal.
3. The brain can recover – but it takes time!
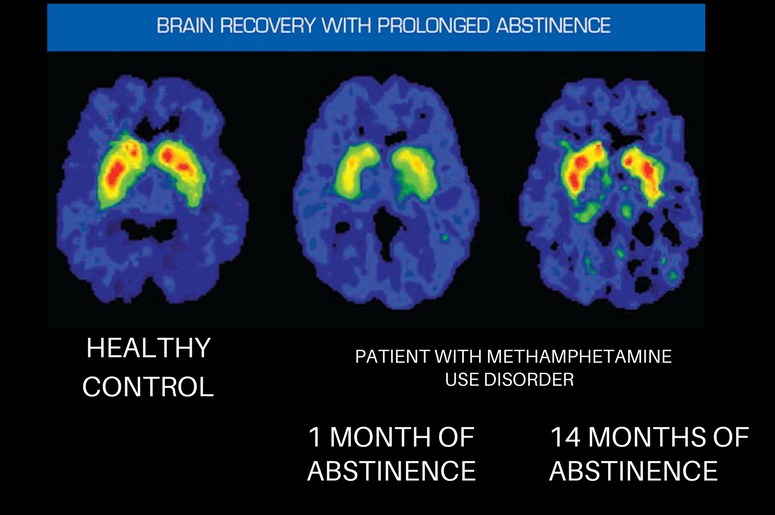
How the brain recovers from addiction is an exciting and emerging area of research. There is evidence that the brain does recover; the image below shows the healthy brain on the left, and the brain of a patient who misused methamphetamine in the center and the right. In the center, after one month of abstinence, the brain looks quite different than the healthy brain; however, after 14 months of abstinence, the dopamine transporter levels (DAT) in the reward region of the brain (an indicator of dopamine system function) return to nearly normal function (Volkow et al., 2001).
There is limited research on the brain’s recovery from alcohol and marijuana use. However, recent studies have shown that some recovery does take place. For example, one study found that adolescents that became abstinent from alcohol had significant recovery with respect to behavioral disinhibition and negative emotionality (Hicks et al., 2012). Lisdahl and colleagues propose that this could mean that some recovery is occurring in the prefrontal cortex after a period of abstinence. Furthermore, other research has found that number of days abstinent from alcohol was associated with improved executive functioning, larger cerebellar volumes, and improved short-term memory.
While promising, this field of research is in its infancy and there have been conflicting results that instead show minimal to no recovery from cognitive deficits. This is especially true for studies evaluating the brain’s recovery from marijuana use, specifically in regards to IQ. On the other hand, some studies have shown that former marijuana users demonstrate increased activation in parts of the brain associated with executive control and attention. Whether this is associated with the compensatory response or brain recovery has yet to be determined.
What is clear is that alcohol and marijuana do have neurotoxic effects and that, to some degree, this damage can be reversed. There is minimal evidence on how we can improve brain recovery from substance use, but emerging literature suggests that exercise as an intervention may improve brain recovery. Physical activity has been shown to improve brain health and neuroplasticity. In previous studies of adults, physical activity has improved executive control, cerebral blood flow, and white matter integrity. While none of these interventions have been done in adolescent alcohol or marijuana users, this approach is promising and should be investigated further.
The Top Tools Being Utilized for Research on the Brain in Recovery
Functional brain measurement techniques:
Methods that provide dynamic physiological information about brain function/activity. Functional imaging techniques allow scientists to measure the contributions of various structures to specific psychological processes (e.g., attention, working memory, etc.). Commonly obtained while participants complete ‘tasks’, functional images offer insight to the brain regions that are activated, or recruited, to perform a given task. Atypical brain function in patient populations can include reduced neural activation or a different pattern of brain activation as compared to healthy control populations.
Structural brain measurement techniques:
Imaging techniques that allow one to examine the brain’s anatomical structure. Structural imaging provides static information, and is analogous to taking a photograph of the brain. These images permit evaluation of gross anatomical abnormalities, including tissue atrophy (i.e., loss of neural tissue) and reduced white matter integrity (i.e., weakened connections between neural structures).Magnetic Resonance Imaging (MRI)Diffusion Tensor Imaging (DTI)
Limitations of brain measurement tools for addiction research:
- High cost of utilizing the technologies within research studies.
- Some neuroimaging techniques require IV injection of a radioactive tracer (e.g., PET scan).
- Some techniques are not suitable for everyone. For example, individuals with metal implants and pacemakers cannot undergo magnetic resonance imaging given the nature with which this image is obtained.
- Research methods must be tailored to imaging requirements. fMRI, for example, is sensitive to physical movement and requires that the individual being scanned remain as still as possible. Therefore, tasks performed during an fMRI scan must not require excessive movement for successful performance.
- Different imaging techniques have varying advantages/disadvantages. Some methods provide better temporal resolution (the accuracy of capturing an image with respect to time), whereas others provide superior spatial resolution (the visual clarity of the image). Although no single technique has perfect spatial and temporal resolution, multimodal imaging techniques (the simultaneous use of 2 or more techniques) are being more commonly implemented and provide a more complete picture of brain structure/function.
